New research from Stanford and the Arc Institute could lead to a new and more effective immunotherapy and help clinicians better predict patient response to existing medicines.
Despite their promise, immunotherapies fail to treat many cancers, including over 80% of some of the most advanced breast cancers. And many of those patients who do respond still experience metastases eventually. New research from Stanford University and the Arc Institute has revealed a better way to predict and improve patient responses.
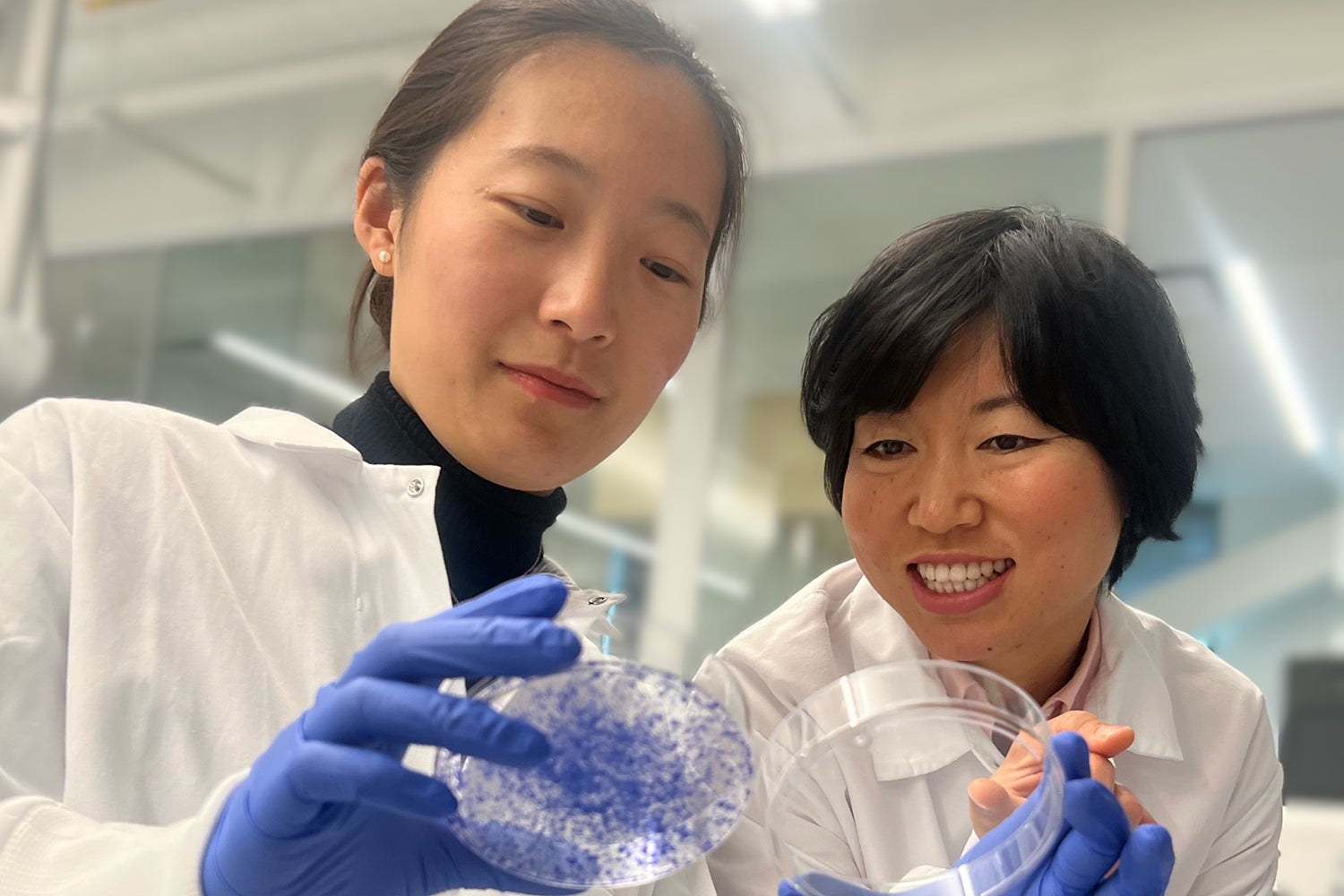
A team led by Lingyin Li, associate professor of biochemistry at Stanford and Arc Core Investigator, found that a protein called ENPP1 acts as an on/off switch that controls breast cancer’s ability to both resist immunotherapy and metastasize. The study, published on Dec. 20 in the Proceedings of the National Academy of Sciences, showed that ENPP1 is produced by cancer cells and by healthy cells in and around the tumor, and that high patient ENPP1 levels are linked to immunotherapy resistance and subsequent metastases. The research could lead to new, more effective immunotherapies and help clinicians better predict patient response to existing medicines.
“Our study should offer hope for everyone,” said Li, who is also an institute scholar at Sarafan ChEM-H.
I’d like mine turned off please